You Inspire The Best in Us.
With the many advances in care and treatments, today’s patients have more and more reasons to expect the best outcomes. Here are the incredible stories of our patients and their journeys. Click on a thumbnail and scroll down to view each story.


Taking a Mulligan
By Tracy H. Stanton
Jay Watson, Head Coach of the Golf Team at Hannah-Pamplico High School, says, “When God gives you a mulligan, take it.”
In the game of golf, a mulligan is defined as a free shot in informal play when the previous shot was played poorly. In other words, it is a do over.
The great golfer Bobby Jones once said, “Golf is the closest game to the game we call life. You get bad breaks from good shots, you get good breaks from bad shots, but you have to play the ball as it lies."
"Having played golf all my life, the game has tested me in the past, but so has life. It’s hard to play it as it lies, and sometimes you have to take a mulligan…or two,” Jay explains.
For 40 years, Jay has worn some type of uniform in his career of protecting others. He served as a volunteer fireman, a soldier in the South Carolina Army National Guard and a sergeant for the Florence County Sheriff’s Office.
In October 2021, he was transporting five COVID-positive inmates to an infusion center when he contracted COVID-19, even though he was vaccinated. His symptoms worsened to the point that on October 15, he was transported by ambulance from his home in Pamplico to McLeod Regional Medical Center, where he was diagnosed with bilateral pneumonia as a result of the infection.
The next day, Jay was put on the ventilator, where he would remain intubated for seven days.
That week was the hardest for Jay’s family. Valeria was at home, also sick with COVID, and Jay’s son Gray and daughter Taylor Anne were unable to visit him because of the COVID restrictions.
They relied on the staff in the Medical Intensive Care Unit (MICU) to keep them informed of Jay’s condition.
“When I was being taken off the ventilator, I thought I was dreaming,” says Jay. “I could hear voices and sounds around me, but everything was dark. The female voices become clearer, and I realized they were calling my name. The sweet pleading voices then turned to cheers and applause as I struggled to open my eyes.”
One of those voices was Johnette Touchberry, the Nurse Practitioner who took him off the ventilator. “What a godsend she and Megan Wallace, the other Nurse Practitioner, turned out to be,” Jay recalls.
“Then she hit me with it – ‘You died, and you came back.’”
Johnette explained that Jay’s heart had stopped for 16 minutes on October 16 due to the sheer volume of fluid from his bilateral COVID pneumonia. Megan and the staff worked to revive him, and he was placed on the ventilator for a week before being taken off on October 23.
He became affectionately known as the McLeod Miracle.
Once Jay was weaned off the ventilator, he remained in quarantine until November 2.
He had no visitors, nor had he seen his family since October 15 while being loaded into the ambulance.
Returning to reality was hard on Jay. He had no strength in his arms and legs, could not hold anything with his fingers or even feed himself, and had lost more than 50 pounds. After being discharged home from McLeod on November 4, he faced a whole new world with an oxygen tank and a walker.
The week of Thanksgiving, Jay had an appointment with McLeod Pulmonologist Dr. Vinod Jona. During the visit, Dr. Jona showed him and Valeria two X-rays: the one taken that day, which showed some scarring in his lungs from COVID, and the one from October 16, where his lungs were filled with fluid. Dr. Jona told them that Jay should not even be here today and had no explanation for his recovery.
On the ride home after the appointment, Jay and Valeria were overcome by emotion. They decided God had given him a mulligan.
Six months after his hospitalization, Jay was playing a round of golf in April with his son Gray and his good friend Brad. As they finished the last hole, Jay felt a spasm in his left arm and side. He assumed it was due to the neurological damage he suffered after his infection and time on the ventilator. After his hand surgery in December 2021, Jay was told some residual numbness could take up to a year to go away.
A week after the spasm, Jay saw McLeod Cardiologist Dr. Alan Blaker for a regular check-up. Before leaving the office, Jay mentioned the incident on the golf course. Dr. Blaker decided to schedule his annual echo and stress test. The results of both were slightly abnormal. Dr. Blaker explained it could be a lingering effect from COVID but decided to schedule a heart catheterization to be sure.
The procedure revealed three blockages. As a result, Dr. Blaker and McLeod Cardiothoracic Surgeon Dr. Cary Huber admitted Jay for three days until the triple bypass surgery could be performed.
This time around, Jay could have visitors, and he spent the days with family and friends and reading his Bible. The day after Jay’s seven-hour open heart surgery, the medical staff told him he would get up and sit in a chair. “Moaning and griping, I did get in that chair, squeezing tight to my chest that little heart shaped pillow. If l learned anything from my experience in October, it was to trust the medical team,” explains Jay.
In June, Jay met with Dr. Huber for a follow-up appointment. No rhythm or valve problems were identified, and there was no heart damage since Jay didn’t have a heart attack. He did learn, however, that his widowmaker artery was more than 93 percent closed in addition to the other two blockages.
“God had given me a mulligan once again,” Jay adds.
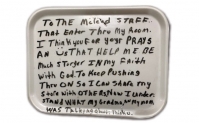
“In Christianity, it’s God who reaches out to us, seeking to throw us a lifeline if we will only respond to His help. For me, that lifeline worked through the hands and hearts of the MICU staff when they brought me back after 16 minutes of no heartbeat, and when they worked to nurture and care for me while I was on the ventilator for seven days. I can never thank them enough.”
Two weeks after his triple bypass surgery, he watched his daughter Taylor Anne graduate from high school.
At the end of 2021, Jay retired from the Sheriff’s Department after 25 years. A month later, he began filling in as a substitute teacher for Florence School District Two. He eventually came out of retirement and returned to the Florence County Sheriff’s Department to serve as the School Resource Officer for Hannah-Pamplico High School.
“In addition, they let me coach the golf team,” says Jay. “If I can touch just one young person’s life in a positive way, then it is all worth it.”
On her husband’s medical journey, Valeria says, “I have seen two miracles firsthand. I am so thankful for the excellent care Jay received from the clinical staff at McLeod. God had him in the right place at the right time with the right people in October 2021 and May 2022.”
In December 2023, Jay and Valeria celebrated their 30th wedding anniversary.
“Valeria’s faith never wavered, both in the Lord Our Savior and in me. She was the rock on which our family stood. She keeps telling me that God isn’t done with me yet. Each day, I believe her more and more.”
Today, Jay says he is a changed person. His physical health is better than it has been in years, and he has a different outlook on life. “McLeod gave me the best care a man could receive.”
He reminds everyone that if God gives you a mulligan, take it. “I did…twice,” adds Jay.
-
McLEOD REGIONAL MEDICAL CENTER FLORENCE
843-777-2000 -
McLEOD DARLINGTON
843-777-1100 -
McLEOD DILLON
843-774-4111 -
McLEOD LORIS
843-716-7000 -
McLEOD SEACOAST
843-390-8100 -
McLEOD CHERAW
843-537-7881 -
McLEOD CLARENDON
803-433-3000



-
McLEOD REGIONAL MEDICAL CENTER FLORENCE
843-777-2000 -
McLEOD DARLINGTON
843-777-1100 -
McLEOD DILLON
843-774-4111 -
McLEOD LORIS
843-716-7000 -
McLEOD SEACOAST
843-390-8100 -
McLEOD CHERAW
843-537-7881 -
McLEOD CLARENDON
803-433-3000
 Find a Doctor
Find a Doctor  Locations
Locations  Services
Services